Why Hospitals Can’t Thrive Without an HCMS
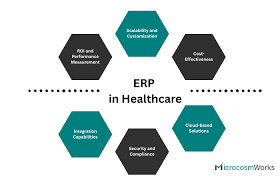
A health care management system (HCMS) is the digital nerve-center that connects patient records, scheduling, billing, analytics and remote monitoring into one secure, real-time platform. In 2025 the stakes are higher than ever: aging populations, tight budgets and new data-sharing laws such as the U.S. 21st-Century Cures Act all demand faster, smarter and more transparent care.
“You can’t call it a digital transformation if nurses still chase paper charts,” says Tamer Badr, CEO of Singleclic. “An HCMS turns raw data into life-saving decisions—without adding clicks to the caregiver’s day.”
People Are Always Asking: “Isn’t an EHR Enough?”
No. An electronic health-record (EHR) is just one module. A true HCMS also:
- Automates admissions, discharge & transfer (ADT)
- Syncs pharmacy, lab and radiology in real time
- Embeds AI alerts for sepsis or drug conflicts
- Integrates billing, insurance clearing-house and patient wallets
- Provides dashboards for quality metrics, ESG and cost per case
Hospitals running a unified system shave 18–22 % off admin overhead and cut medication errors by double digits, according to KLAS and Deloitte market studies.
Market Leaders and What Makes Each Shine
Below is a no-fluff look at eight prominent HCMS/EHR platforms, their standout automations, and where they still trip up.
“We built Singleclic’s stack for hospitals that need bilingual portals, VAT compliance and cloud agility but don’t have Epic budgets,” Badr notes. Explore details ➜ Healthcare Solutions.
Five High-Impact Use Cases You Can Deploy in 90 Days
- Auto-Triage Chatbot
- Collects symptoms, risk factors and insurance info before the patient arrives.
- Collects symptoms, risk factors and insurance info before the patient arrives.
- Smart OR Scheduling
- ML matches surgeons, equipment and predicted turnover time, boosting theater utilisation by 14 %.
- ML matches surgeons, equipment and predicted turnover time, boosting theater utilisation by 14 %.
- Drug–Drug Interaction Alerts
- Real-time pharmacy interface flags conflicts at order entry.
- Real-time pharmacy interface flags conflicts at order entry.
- Claims Denial Prediction
- AI engine scores each claim; risky ones routed for review, cutting write-offs.
- AI engine scores each claim; risky ones routed for review, cutting write-offs.
- Patient Engagement App
- Pushes prep instructions, follow-up surveys and in-app payments; 25 % fewer no-shows on average.
- Pushes prep instructions, follow-up surveys and in-app payments; 25 % fewer no-shows on average.
The Good—And the Gotchas
Major Benefits
- Clinical Accuracy: Physicians see unified data, reducing duplicate tests.
- Operational Efficiency: Automated billing and inventory save millions.
- Regulatory Compliance: Built-in audit trails meet HIPAA/GDPR.
- Data-Driven Strategy: CFOs track cost per DRG or per clinic in real time.
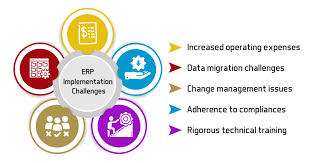
Real-World Drawbacks
- Change Fatigue: Nurses may resist new screen flows—plan extra training.
- Alert Overload: Poorly tuned AI can drown staff in pop-ups (Epic users call it “alarm fatigue”).
- Interoperability Gaps: Competing systems still struggle with flawless FHIR data exchange.
- CapEx Shock: Top-tier implementations run into tens of millions; ROI takes 3–4 years.
Reviews from the Front Lines
Dr Reem H., Chief Medical Officer, Dubai
“Our Epic go-live was painful but worth it—sepsis mortality fell 9 % after the early-warning algorithm.”
Mohamed K., IT Director, Cairo Cardiology Center
“We switched from paper to Odoo with Singleclic’s help. Inventory leaks dropped instantly because every stent scan deducts stock.”
Sarah L., Revenue Cycle Lead, UK private chain
“athenahealth bots now pre-check every claim. Denials are down by a third, but revenue-share costs pinch when volumes surge.”
FAQ—Straight Answers
Q1. How long does a full HCMS rollout take?
Medium hospitals – 9 to 14 months. Academic centers – 18 + months. Single clinics can go live in six weeks with cloud systems.
Q2. Cloud or on-prem?
Cloud accelerates updates, but some regulators require local hosting. Hybrid models (edge caches + cloud analytics) are rising.
Q3. Can AI diagnose patients?
AI supports, not replaces, clinicians. Regulators still mandate human sign-off for critical decisions.
Q4. What about data migration?
Budget up to 25 % of the project for cleansing and mapping legacy records—often the hidden iceberg.
Implementation Checklist
- ✍️ Executive Sponsorship: Secure C-suite champion and clinical lead.
- 📊 KPI Baseline: Track error rates, LOS, claim denials before kickoff.
- 🔐 Security by Design: Role-based access, encryption keys, zero-trust network.
- 🧑🏫 Super-User Program: Train a nurse/doctor in each ward to be the first-line mentor.
- 🔄 Phased Go-Live: Start with outpatient, then inpatient, then ancillaries.
- 📈 90-Day Review: Compare KPIs, tweak workflows, add missing reports.
Looking Ahead—Smart Hospitals & Beyond
The “smart hospital” market—AI, IoT, robotics—could hit $148 billion by 2029. Expect edge devices to stream vitals directly into the HCMS, while 5G enables untethered surgical robots. Interoperability mandates will enforce FHIR APIs, nudging vendors toward open ecosystems.
“Within five years, your hospital bed will message the pharmacy when the drip runs low,” predicts Badr. “An effective health care management system is step one to that future.”
Conclusion—Choose the System That Fits Your Mission
A health care management system is not just another IT project; it’s the core engine of quality, safety and sustainability in modern care. Evaluate platforms on automation depth, usability, interoperability and total cost—not glossy demos. Pair the technology with robust change management, and the payoff is faster diagnoses, lighter admin loads and healthier bottom lines.
Ready to plan your hospital’s digital leap? Explore Singleclic’s end-to-end blueprint ➜ Health-Care Solutions